Beyond the pink ribbon
Facing the complexities of breast cancer

Winship FALL 2016 Moonshot to cure cancer 14 Cassie Mitchell: cancer couldn’t keep her from Paralympic glory 16
On the cover — Angela Yamini was 43 years old when she was diagnosed with metastatic breast cancer. She received chemotherapy before undergoing a lumpectomy and radiation therapy at Winship. Now, two years later, she is in remission and is focused on staying well so she can be there for her family. She is pictured at home with her three daughters: Kira, age 15; Kamryn, age 10; and Kaela, age 18.

Executive Editor: Judy Fortin
Editor: Catherine S. Williams
Art Director: Peta Westmaas
Photographer: Jack Kearse
Production Manager: Carol Pinto
Winship
14
16
IN THIS ISSUE
Winship in the News 2
Wally Curran launches The Winship 80; the Winship Cancer Network expands; celebrating 5,000 bone marrow transplant patients.
Beyond the Pink Ribbon 6
One size does not fit all when treating breast cancer. The interdisciplinary approach of the Glenn Family Breast Center offers the best options to every patient.

The Cancer Moonshot 14
Vice President Biden challenges cancer researchers to double the rate of progress against cancer in the next five years. Here’s how Winship is responding.

Emory | Winship Magazine is published biannually by the communications office of Winship Cancer Institute, a part of the Woodruff Health Sciences Center of Emory University, emoryhealthsciences.org. Articles may be reprinted in full or in part if source is acknowledged. If you have story ideas or feedback, please contact judy.fortin@emory.edu. © Fall 2016. Website: winshipcancer.emory.edu. To view past magazine issues, go to winshipcancer.emory.edu/magazine.
You Inspire Us
16
Four patients whose amazing feats make us say, Wow!

Champion for Lung Cancer Research 21
Bill Maiola was determined to make a difference in lung cancer research.
Why I Run 22
A few of the people who embody the spirit and enthusiasm of the Winship Win the Fight 5K.
Point of View: When cancer comes back 24
Wendy Baer shares advice for patients facing cancer again.
Emory University is an equal opportunity/equal access/affirmative action employer fully committed to achieving a diverse workforce and complies with all federal and Georgia state laws, regulations, and executive orders regarding nondiscrimination and affirmative action. Emory University does not discriminate on the basis of race, age, color, religion, national origin or ancestry, sex, gender, disability, veteran status, genetic information, sexual orientation, or gender identity or expression.
2016
FALL
“You can cry about it or do something about it.”
—Cassie Mitchell Paralympian, Biomedical engineer
16-WINSHIP-0181 6
VIce President Joe Biden addressing the Cancer Moonshot Summit
OUR PAST IS OUR PROLOGUE
Winship Executive Director Dr. Wally Curran calls for The Winship 80
The Winship 80 are patients who put their lives in our hands, scientists dedicated to unlocking the code of cancer, philanthropists who provide the support needed to create new knowledge, community leaders, caregivers, advocates, and volunteers who have shaped Winship Cancer Institute.

ONE YEAR FROM NOW WE WILL CELEBRATE THE 80TH ANNIVERSARY OF THE FOUNDING OF WINSHIP CANCER INSTITUTE. In 1937, Robert Woodruff, the president of Coca-Cola, lost his mother to cancer. He was determined that no one would have to leave the state of Georgia to receive the best cancer treatment. In her honor, he gave a generous gift to Emory University that helped create the Robert Winship Memorial Clinic, named for Woodruff’s maternal grandfather.

Today, we are fulfilling Mr. Woodruff’s mission by translating research discoveries into better cancer care and making the most advanced cancer care available right here in Georgia. Looking back over the past eight decades, we see evidence of our hard work in the number of patients we care for from throughout Georgia and beyond, in the complexity of cancers we tackle, in the scientific contributions we make on a truly
global scale, and in our ongoing commitment to lessen the burden of cancer in the state of Georgia.
There are thousands of people over Winship’s 80-year history who have made this happen and as part of our anniversary commemoration, we will honor 80 of them. The Winship 80 are patients who put their lives in our hands, scientists dedicated to unlocking the code of cancer, philanthropists who provide the support needed to create new knowledge, community leaders, caregivers, advocates, and volunteers who have shaped Winship Cancer Institute. Please let us know who you think should be one of The Winship 80.
We invite you to submit a nomination online and tell us how that person has made a difference. For more information and to fill out a nomination form go to winshipcancer. emory.edu/Winship80-nomination. The deadline is Dec. 2, 2016.
2 Winship Magazine | winshipcancer.emory.edu winship | in the news
Robert Woodruff, founder of Winship Cancer Institute, and his mother Emily Winship Woodruff.
KAY HINTON
Owonikoko Receives Leadership Award
Winship medical oncologist Taofeek Owonikoko is one of 13 recipients of the 2016 National Cancer Institute Clinical Investigator Team Leadership Award.

The prestigious award recognizes and supports outstanding mid-career clinical investigators at NCI-designated cancer centers who are significantly engaged in NCI-funded multi-center clinical trials. Owonikoko receives the award for his leadership of innovative work in lung cancer, thyroid cancer, and other aerodigestive-tract cancers.
The award supports Owonikoko’s ongoing work in clinical trials, including his leadership on two investigator-initiated trials that promote patient access to novel therapies. W
NAVICENT JOINS CANCER NETWORK
ACADEMIC CHAIRS, PROFESSORSHIP HONOR WINSHIP RESEARCHERS
Winship Cancer Institute has named three key leaders to fill endowed positions. Suresh

S. Ramalingam will hold the Roberto C. Goizueta Chair for Cancer Research; Mylin
A. Torres will hold the Louisa and Rand Glenn Family Chair in Breast Cancer Research; and Bassel F. El-Rayes will hold the John Kauffman Family Professorship for Pancreatic Cancer Research. An academic chair or professorship recognizes extraordinary achievement and leadership and is invaluable for recruiting and retaining top faculty members. Endowment income from an academic chair contributes to the recipient’s scholarly work and professional activities. W
The Peyton Anderson Cancer Center at Navicent Health in Macon, Georgia, is the second hospital outside of Emory Healthcare to join the Winship Cancer Network. The partnership will allow Navicent, the second largest hospital in the state, to collaborate with Winship and provide its patients with access to innovative cancer research and treatment. The Winship Cancer Network was launched in January 2016 when Archbold Memorial Hospital in Thomasville became the inaugural member. W
Winship Magazine | fall 2016 3
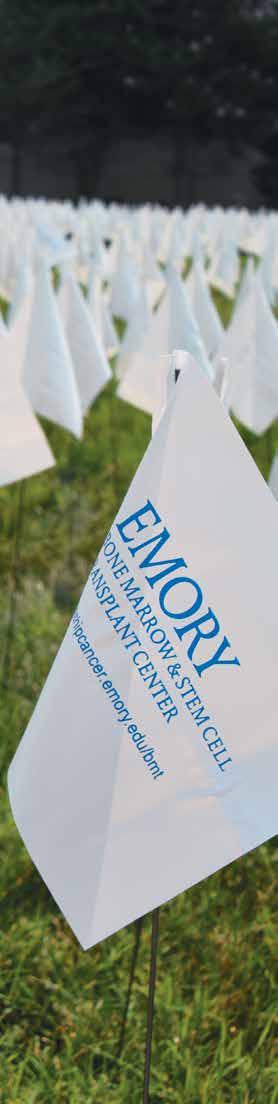
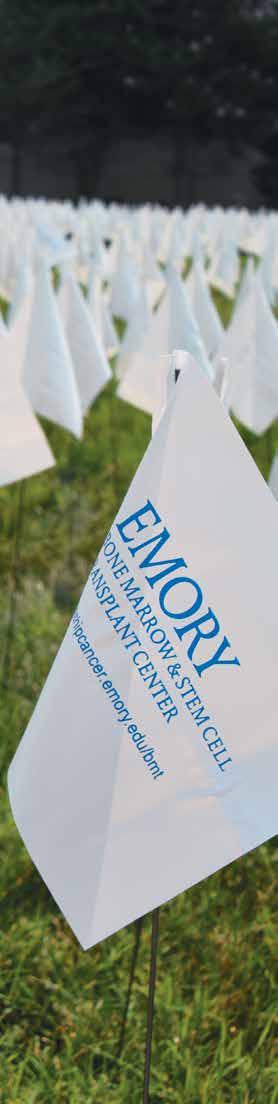
5,000 FLAGS = 5,000

The Bone Marrow and Stem Cell Transplant Center at Winship Cancer Institute hit a milestone this spring when Glenn Pontoo became the 5,000th patient to receive a bone marrow or stem cell transplant. Pontoo, a multiple myeloma patient, was transplanted on June 20. The very next day, he came down from his hospital room to the School of Medicine lawn to take part in the celebration and plant the 5,000th flag.
A week earlier, BMT nurses, patients, doctors, research coordinators, hospital staff, volunteers, and other Winship friends planted 4,995 flags on the lawn to represent all the patients to date. On June 21st, an enthusiastic crowd came to celebrate and plant the last five flags, including some of Winship’s earliest transplant patients, such as Joyce Wilson (transplanted in 1981) and Ronnie Hyatt (transplanted in 1982). BMT recipients held up signs with


PATIENTS
the year of their transplants and joyously reunited with doctors and nurses who had cared for them.

Winship’s Bone Marrow and Stem Cell Transplant Center was one of the first of its kind in the country when it started transplanting patients with blood cancers and blood disorders in 1979. It started with two hematologists who saw the potential of this new treatment: Elliott Winton, still a practicing physician and researcher with the Winship hematology team, and retired hematologist Ralph Vogler.
“This is death-defying treatment. If we can cure somebody, particularly somebody with many years left of good quality of life, that’s one of the biggest thrills of my career,” says Winton.
Visionary leaders, researchers, and nurses grew the program over its 37-year history into a center that now performs this life-saving procedure for over 430 patients a year.
 By Catherine Williams
By Catherine Williams
4 Winship Magazine | winshipcancer.emory.edu
3D imaging improves biopsy process


Emory inaugurated 3D mammography, or digital breast tomosynthesis (DBT), imaging technology for regular screening mammograms because it is more accurate at detecting breast cancers and produces fewer false-positives that result in patient call-backs. But when a woman is called back and additional mammograms show something that could be cancer, the next step is a biopsy to sample a tiny bit of tissue from the suspected area. Every stage of this process, and any subsequent treatment, is extremely dependent on accuracy. Now, doctors within Winship’s Glenn Family Breast Center are using 3D technology throughout the screening and biopsy process. Some breast lesions and calcifications may be subtle and visible only on 3D imaging, so using the technology to guide biopsies enables physicians to more accurately pinpoint and mark areas that may prove to be small, treatable breast cancers. The new Affirm 3D biopsy system is being used at Winship breast imaging facilities on Emory’s Clifton Campus, Emory University Hospital Midtown, Emory Johns Creek Hospital, and soon will be at Emory Saint Joseph’s Hospital. W
Winship Magazine | fall 2016 5
Michael Cohen is director of Emory Breast Imaging Centers.
feature | breast cancer
Baby Derin was a surprise blessing, born less than a year after Deja Er was diagnosed with triple negative breast cancer and only five months after she completed radiation therapy treatments at Winship. Mother and son are thriving.

6 Winship Magazine | winshipcancer.emory.edu
Facing the complexities of breast cancer
 BY Quinn Eastman
BY Quinn Eastman
Kristen Sheubrooks
(above)
was
34 years
old, the mother of a boy in preschool and a baby girl, when she received a diagnosis of metastatic breast cancer. She knew she was at high risk for the disease, but the timing seemed especially horrible, she says. “We had to explain that Mommy would be tired a lot, and that my hair would look different,” Sheubrooks says. Women who are diagnosed with breast cancer before the age of 50 are usually recommended to undergo genetic testing. Sheubrooks did not need to struggle with this decision. Since her mother had breast cancer twice, Sheubrooks and her sister had been tested already and both were found to be brca carriers.
Winship Magazine | fall 2016 7
She had been having regular preventive screenings, alternating MRI and mammogram, every six months since her 20s. A second pregnancy in 2014 broke up that routine. When her daughter was five months old, she felt a lump in her breast. While getting it checked, she learned that a spot also had been detected on her liver.
Her local Georgia doctors recommended that she come to the Glenn Family Breast Center at Winship and enroll on a clinical trial designed specifically for BRCA carriers with metastatic breast cancer. Doctors she consulted in New York advised the same thing. The trial is testing an experimental drug called veliparib, in combination with two standard chemotherapy drugs, carboplatin and paclitaxel. Researchers think that BRCA-linked cancers, in particular, may be more sensitive to this drug.
When Sheubrooks started on chemotherapy, it felt like “the worst stomach flu you can imagine, times ten,” she says. But anti-nausea medications helped and later her drug regimen was adjusted to allow for the least toxicity while she remains on the study.

Sheubrooks does not know whether she has been receiving veliparib, rather than placebo, but she is willing to guess that she has, because her response to the medication regimen
was so dramatic. The lump in her breast is now undetectable, while the spot on her liver has been barely detectable for a few months, she reports.
Women who are diagnosed with breast cancer before the age of 40 tend to develop more aggressive cancers. And BRCA1 carriers are more likely to develop triple negative breast cancer (see definition on page 12). These are complicating factors doctors know about. But every woman fighting breast cancer faces choices.
The care teams at Winship’s Glenn Family Breast Center have the experience and training to advise women on the choices they must make, and to design treatment regimens for their unique circumstances. This article examines some of the complexities that can shape a woman’s encounter with breast cancer.
African-American women diagnosed with breast cancer in Georgia have a higher mortality rate than white women do, and access to mammograms is thought to play a role. See sidebar on page 11.
8 Winship Magazine | winshipcancer.emory.edu
Tracey Monday was diagnosed with breast cancer at the age of 26.
Youth
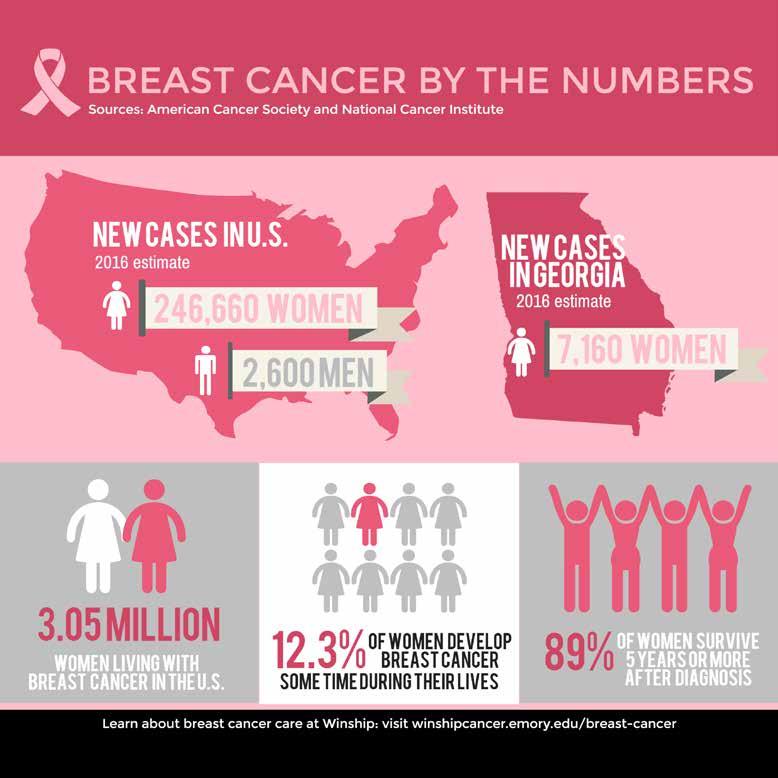
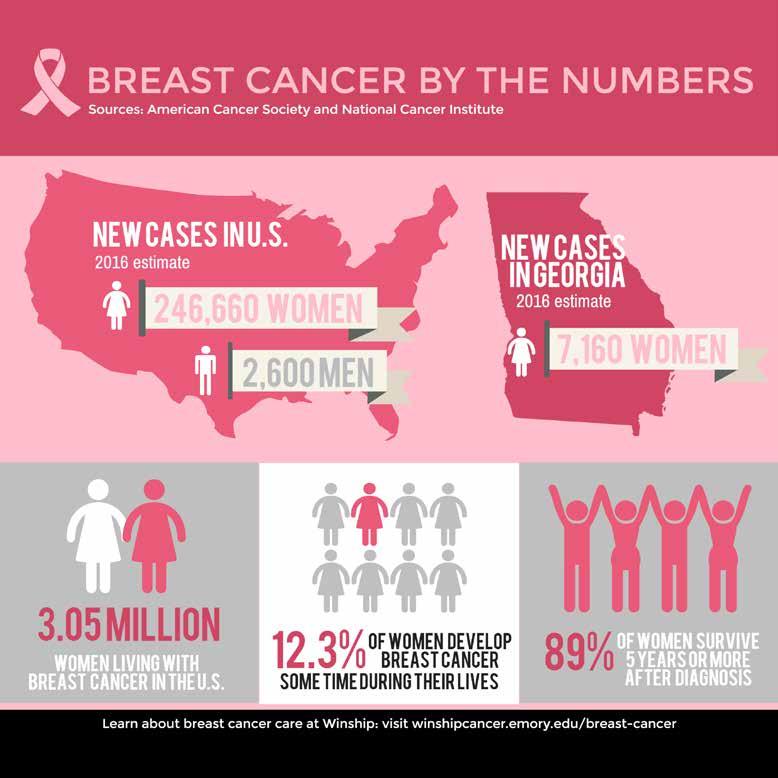
Breast cancer in women younger than 40 makes up less than five percent of all cases diagnosed in the United States, but this group has made up nine percent of Winship breast cancer patients in the last two years. Most young women do not get annual mammograms, so these cancers tend to be more advanced due in part to the fact that they go undetected until a patient or physician feels a lump during a physical exam. Even when comparing cancers at the same stage, breast cancers that occur in younger women tend to be less likely to be treatable with hormone therapy, and have a higher risk of recurrence and metastasis.
Breast cancer treatment in younger women also brings with it unique concerns. Chemotherapy as well as endocrine therapy (such as tamoxifen) can affect ovarian function, resulting in irregular periods and contributing to early menopause. That cuts into time a woman may have planned for pregnancy and childbirth. Early menopause can affect a younger woman’s health in other ways, such as reduced bone density.
“Our team approach can provide benefits to women who have these needs,” says Mylin Torres, a radiation oncologist and director of the Glenn Family Breast Center at Winship. “We make sure they have quick access to fertility consultation, genetic counseling, or a plastic surgeon, so there’s minimal delay in starting their cancer treatment.”
Winship oncologist Jane Meisel describes a patient in her 20s, whom she advised to consider measures to preserve fertility. The patient began crying and said that two other doctors she had visited had not brought up the topic.
“These are the patients who keep me up at night,” Meisel says.
Winship patients who need a consultation on fertility can usually obtain an appointment within 24 hours, says Jessica Spencer, medical director of Emory’s Reproductive Center. Options include egg or embryo preservation, drugs that may be able to reduce the ovaries’ exposure to chemotherapy, and alternatives such as adoption or surrogacy.

In addition, younger women diagnosed with breast cancer are advised that they should undergo genetic testing for BRCA1
and BRCA2 mutations. While BRCA1 and BRCA2 mutations are rare in the general population (estimated at 1/400 to 1/800 women), the relative likelihood goes up when someone has breast cancer at a young age.
For Tracey Monday, who was diagnosed with breast cancer when she was just 26, the question of genetic risk had some sharp teeth, because her mother had undergone treatment for ovarian cancer just a couple of years before. As Monday was preparing to start chemotherapy, her mother’s cancer came back. Her genetic testing did turn up a BRCA variant, but it was not identified as a contributor to breast cancer risk.
A recent survey of young breast cancer survivors throughout Georgia, conducted by Winship genetic researcher Cecelia Bellcross and colleagues, found that only half reported being referred or recommended for genetic counseling. A companion survey of Georgia doctors also found gaps in health providers’ understanding of breast cancer genetic risk, says Bellcross, who has developed online tools to help women decide whether to undergo genetic testing.
“Many women think: ‘I’ve already had breast cancer. What difference does it make?’” says Bellcross. “What they don’t realize is that with BRCA, there’s an increased risk of a second breast cancer, or ovarian cancer. They don’t want to have to go through this a second time.”
Chemo for one, planning for two
Pregnancy has a complex relationship with breast cancer risk. The hormones of pregnancy, such as estrogen, are thought to speed up breast cancer growth, although having children early in life also lowers the risk of developing breast cancer later. Studies indicate that pregnancy does not boost the risk for BRCA1 carriers, like Kristen Sheubrooks. And in particular, her cancer was triple-negative, an aggressive type insensitive to both estrogen and estrogen deprivation.
Sometimes a breast cancer diagnosis interrupts a woman’s family planning in a more direct way. After giving birth to her daughter in 2014, Patricia Jean detected a lump in her breast. Her
Winship Magazine | fall 2016 9
Reetu Earp discusses options with her doctor, Jane Meisel.
“Attitude gets you through,” says patient


10 Winship Magazine | winshipcancer.emory.edu
and Winship Advisory Board member Sandra Jackson (right), pictured here with daughter Jenna.
Pamela Bryant, her mother Juanita Bradley, and aunt Jennie Williams, are all breast cancer survivors. Bryant went on a clinical trial that cut the length of her radiation treatment in half.
gynecologist scheduled her for an ultrasound and biopsy, and as part of a standard screening process, she had a pregnancy test.
“I had a few days to be happy about the pregnancy,” says Jean, an accountant for a communications company. “When I came in to learn the biopsy results, I did not expect to hear bad news, so I was stunned and very concerned.”
The biopsy results indicated possible stage II cancer. It was HER2-positive (see definition page 12), a type of breast cancer that tends to be more aggressive. The Atlanta-area surgeon and oncologist she was initially referred to were eager to begin treatment, but they strongly recommended that she terminate her pregnancy, just five weeks along.
“I thought that would be a horrible thing,” she says.
Instead, Jean wanted to explore the possibility of delaying chemotherapy until the second trimester. Her surgeon and oncologist resisted.
Chemotherapy drugs are thought to be most harmful to the fetus during the first trimester of pregnancy. However, in several retrospective studies, commonly used chemotherapy drugs given in the second or third trimester do not increase the risk of birth defects.
Praying and searching for options, she read a news article about a pregnant woman who was treated for breast cancer in New York. She called that woman’s doctor and was squeezed in for an appointment that week.
Doctors in New York reassessed her case and developed a plan: surgery in New York, followed by chemotherapy during the second trimester of her pregnancy in Atlanta. Jane Meisel, an oncologist in the Glenn Family Breast Center who had done research on pregnancy-associated breast cancer treatment, agreed to take her on as a patient. Treatment with trastuzumab was delayed until after the baby’s birth because of its previously reported interference with amniotic fluid production, Meisel says.
Surgery went well, but chemotherapy during pregnancy was grueling, Jean says. She remembers tears coming to her eyes when she watched the Winship nurses handling red-colored doxorubicin with gloves.

Jean’s son was born in April 2016, close to full term and in the normal weight range. Afterwards, she started a year-long treatment with trastuzumab. She says she does not regret her decisions.
“I did a lot of research. I read about both disasters and successes,” she says. “I am not worried, but I am aware. There are risks we have to live with. God helped me through every step of my journey.”
Bringing better care into the community
Black women diagnosed with breast cancer in Georgia are 29 to 32 percent more likely to die from this disease than white women diagnosed with breast cancer in Georgia. This disparity can be attributed to some biological factors, such as black women being diagnosed with more aggressive subtypes of breast cancer, but access to screening and quality care may play a role. Under the direction of Winship’s Sheryl GabramMendola, surgeon-in-chief at Grady Memorial Hospital, a partnership between the Glenn Family Breast Center at Winship and the Avon Foundation Comprehensive Breast Center was formed at Grady to provide better breast health services to women in underserved communities served by Grady. The Avon Breast Center has a multidisciplinary program offering clinical and support services, including screening, diagnoses, treatment, genetic counseling, patient navigation, and laboratory services. Through this initiative, the Avon Breast Center has been able to detect more earlystage breast cancers, reduce the number of women with latestage diagnoses, and improve access to screening services in this community. W
Winship Magazine | fall 2016 11
feature | breast cancer
Breast cancer terms defined*
BRCA: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. Inheriting a BRCA1 mutation raises the lifetime risk of breast cancer in the range of 55 to 65 percent. For BRCA2 mutations, the risk is around 45 percent.
HER2-positive: Breast cancer cells are tested to see if they have estrogen and progesterone receptors and the growthpromoting protein called HER2. About 1 of 5 breast cancers have too much HER2 and are referred to as HER2-positive.

Triple-negative: If the breast cancer cells don’t have a significant amount of estrogen or progesterone receptors and not much HER2, they are called triple-negative. Triplenegative breast cancers tend to grow and spread more quickly than other types of breast cancer.
*Source: American Cancer Society. For more breast cancer terminology and definitions, go to cancer.org.
Recurrence, more options
Once estrogen-responsive breast cancers relapse, they can be difficult to treat. Sandra Jackson, who was first treated for her breast cancer in 2012, has been taking a drug combination recently approved by the U.S. Food and Drug Administration that goes beyond hormone therapy. Her regimen includes the drug palbociclib, which targets enzymes researchers think drive tumor cell proliferation.
Jackson says one of the key lessons she absorbed from her first experience with breast cancer was: “Attitude gets you through.” She and her family did plenty of research, mapping out the options on a white board at their home, but she also avoided reading too much about possible side effects of the medicines she would take.
“I didn’t want to train my brain to anticipate those experiences,” she says. “But I did rest. I didn’t try to push through it all.”
The second time around, the tumor is so far being held at bay. Jackson remains focused on her young, accomplished
daughters: one a lawyer, the other a university sports recruiter. “Graduations, weddings, what’s the next step?”
Choices
If a woman is facing a breast cancer that has spread to the lymph nodes, oncologists often recommend pre-operative, or neoadjuvant, chemotherapy. This can increase the surgical options for women who would need a mastectomy if they had surgery first, and allow doctors to gauge the cancer’s response to the specific drugs chosen.
A series of ambiguous mammograms in 2015 led Angela Yamini, then 43, to come to the Glenn Family Breast Center at Winship. She learned she had stage III cancer, with some lymph node spread. Yamini, who works at a big technology company, says her first thought was of her husband and three daughters: “I could not leave them. I had to be there for them.”
The cancer cells were faintly estrogen receptor-positive, so her team, led by oncologist Keerthi Gogineni, made a decision to treat it like a more aggressive triple negative cancer. In her case, chemotherapy eliminated signs of cancer from her lymph nodes by the time of surgery.
Instead of having the entire breast removed, she opted for lumpectomy with radiation. At the same time as the lumpectomy, Yamini also was able to have oncoplastic reduction, a plastic surgery technique in which the breast unaffected by cancer is reduced slightly to match the one where the tumor was.
“I had a number of conversations with [Winship surgeon] Dr. Styblo with notebook in hand, talking about the different options,” she says.
Yamini was able to choose the less radical surgery, knowing that recurrence rates for both procedures were approximately the same, Gogineni says. Yamini appreciated getting the information she needed to make treatment decisions.
During her treatment, Yamini’s colleagues brought her meals, and she worked at home. Now she is back to her regular work and home life and taking tamoxifen to reduce the risk of cancer recurring. She says she has some fatigue but is feeling more like herself again.
“Cancer is in the rearview mirror,” she says. “I’m stronger every day.” W
12 Winship Magazine | winshipcancer.emory.edu
Angela Yamini with her doctor, Keerthi Gogineni.
Decoding Genes, Boosting Quality of Life for Breast Cancer Survivors
BY Michelle Hiskey
The survival rates for breast cancer are high, and many American women are living decades beyond their diagnoses. Because so many women survive breast cancer, Winship researchers and physicians are focusing on improving the quality of life for them. A third of breast cancer survivors face serious side effects such as fatigue, depression, and surgery- and radiationinduced breast and skin problems, which can be so devastating that some women consider them worse than their breast cancer treatment. What if doctors could predict the patients who are most likely to suffer post-treatment problems?
The Glenn Family Breast Center at Winship is answering that question through research discoveries that are a direct result of philanthropy.

Chemotherapy works by damaging the DNA in cancer cells but it also leaves an imprint on the DNA of a patient’s blood cells. Studies have linked genetic changes caused by chemotherapy to inflammation, which is considered a major cause of symptoms like fatigue. Research undertaken by the Glenn Family Breast Center has taken that one step further and is the first to identify the connection between chemotherapy and the way genes in non-cancerous blood cells turn on or off to cause inflammation.
“Through these discoveries, we are closer to predicting who will experience fatigue, depression, cognitive dysfunction, skin toxicities, and other morbidities, and we can determine how to fix problems through traditional and alternative treatments,” says Mylin Torres, director of the Glenn Family Breast Center and newly
named recipient of the Louisa and Rand Glenn Family Chair in Breast Cancer Research.
Identifying a genetic marker related to persistent inflammation could benefit patients through treatment strategies and follow-up care designed to minimize side effects.
Torres, a radiation oncologist who has studied fatigue in breast cancer survivors, leads this research with Andrew Miller, William P. Timmie Professor of Psychiatry and Behavioral Sciences, whose research focuses on inflammation and chronic diseases. Torres and Miller joined forces with support from the Cooper Family Foundation, which was attracted to the possibility of meaningful improvements for breast cancer survivors and began giving in 2006.
“We started from nothing and grew and grew,” Miller says. “The Coopers’ funding was the push in that direction.”
Discovery funding like the Coopers’ enables promising ideas to get off the ground and attract highly competitive funding from the National Institutes of Health, Susan G. Komen, American Cancer Society, and Radiation Therapy Oncology Group (now part of NRG Oncology).
“Extramural funding helps us make innovative discoveries, get on the map of the cancer world, and attract national and international leaders to Winship,” says Torres. “Advancing the field of breast cancer by conducting practice-changing research is the mission of the Glenn Family Breast Center.” W
Winship Magazine | fall 2016 13
Glenn Family Breast Center providers, researchers, and Glenn family members. Left to right: Christine Stanislaw, Heather Pinkerton, Sheryl Gabram-Mendola, Paula Vertino, Louisa Glenn D’Antignac, Lou Glenn, Mylin Torres, Uma Krishnamurti, Keerthi Gogineni, Preeta Subhedar.
THE CANCER MOONSHOT

When President Obama delivered his final State of the Union address in January, he charged Vice President Joe Biden with making a decade’s worth of advances in fighting cancer in just five years. The Cancer Moonshot, as it is called, comes at the right time, says Winship’s Executive Director Walter J. Curran, Jr. “Had a president announced this 10 or 20 years ago, I think cancer researchers’ optimism about how much we could do in the final year of a presidency would not be anywhere near the level it is now.”
In June, Curran presided over a standing room only crowd during a special Cancer Moonshot Summit at Winship that attracted more than 100 clinicians, researchers, advocates, public health experts, survivors, caregivers, and even a former NFL linebacker. The event was one of


10 regional summits held across the country at the same time that the Vice President convened a session in Washington, DC.
Set up at roundtables, the attendees tackled tough questions like how to unleash the power of big data on medicine, how to improve
delivery of care to underserved communities, and how to spur more scientific discoveries in cancer. The final recommendations from the Winship group were shared at the end of the Summit and later with the White House Cancer Moonshot Task Force.—
By Judy Fortin
14 Winship Magazine | winshipcancer.emory.edu
The Moonshot is a chance to come together and make a commitment that everyone can benefit equally from what we know.
The Cancer Moonshot makes it clear that we have to have a sense of urgency in tackling this disease.
Our time is now.
We’re at a tipping point in terms of bolstering research and care advances.
Clinical trials are a way to bring people together to exchange the latest knowledge and help move the standard practices to every part of the state.
The big issues are access, affordability, and awareness. Early detection and proximity to care are big concerns for a lot of people.

If we have the ability to transfer money from our bank accounts to others via our phones, why can’t we take the same approach in data sharing for cancer care?
We should bring cloud-based technology for data management and data storage into the medical arena.






The problems tackled by the Cancer Moonshot will be solved in rooms just like this.

Winship Magazine | fall 2016 15
Pamela Roshell, Director, Health and Human Services Department Division IV
Suresh Ramalingam, Winship Deputy Director
Richard Wender, Chief Cancer Control Officer, American Cancer Society
Chris Draft, former NFL player
Lex Gilbert, colon cancer survivor and Winship volunteer
Donald Harvey, Winship Phase I Unit Director
Sagar Lonial, Chief Medical Officer, Winship Cancer Institute
Kim Kerstann, Winship Senior Director for Research Administration
Wow!
Ten days before she was to compete in trials to qualify for the 2016 USA Paralympic team, Cassie Mitchell was in the hospital recovering from pneumonia, tachycardia, and shingles, all side effects of the chemotherapy she was getting to treat chronic myeloid leukemia (CML). Although Mitchell has faced down health problems her whole adult life, she admits she had a moment of doubt.
At age 18, Mitchell was diagnosed with neuromyelitis optica (Devic’s disease), an autoimmune disease of the central nervous system that paralyzed her from the waist down and continued to cause additional upper body and eyesight impairments. She focused energies on college, took up wheelchair sports, and went on to get her doctoral degree and become a research faculty member in the Coulter Department of Biomedical Engineering at Georgia Tech and Emory.
At the same time, the consummate athlete has been racking up world records in track and field events. Despite the leukemia diagnosis in April, she was determined to compete in the 2016 Paralympics. She says her doctor, Winship hematologist Vamsi Kota, supported her.
“I know he has my health as the number one concern, but he also respects my athletics,” says Mitchell, who thanks her entire health care team for their care and encouragement.
Mitchell wore the USA colors to Rio in September and came home triumphant: a bronze medal and personal best in the club throw, and a silver medal and personal best in discus throw.
 CASSIE MITCHELL PARALYMPIAN, BIOMEDICAL ENGINEER
CASSIE MITCHELL PARALYMPIAN, BIOMEDICAL ENGINEER
16 Winship Magazine | winshipcancer.emory.edu
“YOU CAN CRY ABOUT IT OR DO SOMETHING ABOUT IT.”

Winship Magazine | fall 2016 17 YOU INSPIRE US
“EVERYBODY HAS A TREE STORY.”
Neil Norton’s tree story is about how his life changed course on March 19, 1998—the day he received a bone marrow transplant.
At 34, Norton was married and working long hours at his telecommunications business when a leukemia diagnosis put the brakes on his forward momentum. A bone marrow transplant offered him his best chance at a cure and, luckily, an unrelated donor match was found through the bone marrow registry. Still, recovery was long and rough. His wife Lynne was constantly at his side and Winship nurses kept encouraging him. One nurse in particular urged Norton to think of a positive mental image that would help him heal.
Norton had always loved trees, so he imagined the new cells taking root in his bone marrow, growing like a tree. He spent weeks in the hospital imagining trees and after getting out, he turned the images into reality by becoming a certified arborist. Now he spends his days looking long and hard at trees, seeing what most of us miss and, in his words, “staying rooted.”
NEIL NORTON ARBORIST

18 Winship Magazine | winshipcancer.emory.edu YOU INSPIRE US
“I PRAYED FOR STRENGTH AND GOD WAS LISTENING.”
Walter Hawkins thought he might never walk again. The 30-year Navy veteran faced his stage IV lung cancer diagnosis head on and was determined to keep fit throughout treatment, but in December of 2015, a few months after surgery to remove a tumor on his spine, a compression on his spinal cord paralyzed him from the waist down.

Undaunted, Hawkins threw himself into rehab, first pushing himself through the hospital hallways in a wheelchair and later walking with canes. Discipline and setting goals have served Hawkins throughout his life. So, with encouragement from his surgeon Daniel Refai and oncologist Rathi Pillai, he set his sights on walking the Peachtree Road Race in July. Training with his wife Paulina, he worked his way up half-mile by half-mile until he could walk a full 10K (6.2 miles) without stopping. On July 4th, Walter and Paulina finished the race together.
Hawkins says Paulina and his doctors have been with him every step of the way: “They don’t have ‘quit’ in them.”
Winship Magazine | fall 2016 19
YOU INSPIRE US
WALTER HAWKINS NAVY VETERAN
“CANCER TAUGHT ME HOW QUICKLY LIFE CAN CHANGE.”
Emily Schillinger was just 14 years old when she was diagnosed with an ovarian germ cell tumor. Over the next year, she was in and out of Emory University Hospital receiving treatment from Winship doctors. High-dose chemotherapy was followed by a stem cell transplant at Children’s Healthcare of Atlanta.
Now, more than 20 years later, she has no evidence of the disease. After college, Schillinger moved to Washington, DC, and worked with some of the most powerful people in government. She served in the White House press office during the Bush administration, was press secretary to former House Speaker John Boehner, and is now communications director for the House Ways and Means Committee.
“Cancer will shape you forever, but it doesn’t have to define you for the rest of your life,” says Schillinger. “Every year you are blessed to stay healthy is another year you can create something new and change your life in enriching, unexpected ways.”
Schillinger and her husband, Ian, are planning to adopt a baby.


20 Winship Magazine | winshipcancer.emory.edu
Winship Survivorship Program Director Joan Giblin (standing far left) attended Schillinger’s wedding three years ago. Seated are (left to right) Schillinger’s oncologist, William McGuire, mother Cindy Lawrimore, and father Marshal Lawrimore.
EMILY SCHILLINGER COMMUNICATIONS DIRECTOR U.S. HOUSE WAYS AND MEANS COMMITTEE YOU INSPIRE US
CHAMPION FOR LUNG CANCER RESEARCH
BY Marlene Goldman
Bill Maiola was an unstoppable warrior. He never wanted to hear “no” or that something couldn’t be done.
The biggest challenge of his life came in April 2012—one week before his daughter’s wedding—when he was diagnosed with stage IV lung cancer. He had never smoked, there was no family history of cancer, and the 64-year-old exercised regularly and watched his diet.
Maiola defied the odds for almost four years. During that time he and Grace, his wife and cheerleader for 46 years, decided not only to get the “best-of-the-best” care, but also to change the future for others.
“Being in a research institute like Emory is exactly what a cancer patient needs,” says Grace. “You have access to the most brilliant people dealing with the most cutting-edge medicines and access to clinical trials and the latest treatments.”
Inspired by his care team and the groundbreaking research at Winship, the couple created the Maiola Family Fund for Lung Cancer Research.

“Supporting research goes much further than Emory,” she notes. “We were grateful for what we had, and we wanted to be part of the solution. That’s how Bill thought in life—solutions.”
“Bill was one of the nicest human beings I’ve ever met,” says Winship Deputy Director Suresh Ramalingam, who, with his predecessor Fadlo Khuri, treated Bill Maiola and became his friend and admirer. “Together, Grace and Bill fought his diagnosis with an optimism and strength
that moved me. They shared a dedication to championing funds for lung cancer research that will help all families faced with this disease, not just their own.”
Early treatment held Bill Maiola’s tumor in check. When the tumor began growing again, Maiola was among the first U.S. volunteers for a human trial of a targeted medication called AZD9291.
He was in the right place at the right time. Ramalingam was one of two lead
U.S. investigators for the international trial, which subsequently confirmed that the drug could shrink tumors and improve patient outcomes. The FDA has since approved the drug.
Bill Maiola rallied for almost two years before his body developed resistance to AZD9291.

Gifts like the Maiolas’ are critical. Historically, funding for lung cancer research has lagged behind other cancers and has not kept pace with the magnitude of the problem, says Ramalingam.
Bill Maiola’s grand strategy is already showing results. The fund has raised more than $320,000 from family, friends, and former colleagues at the Coca-Cola Company, which matches employee contributions. Those “seed dollars” are particularly welcome because early support for promising ideas is key to securing major grants from the National Cancer Institute and other funders. In one such project, Emory researchers developed a new approach to block mechanisms in tumors that lead to drug resistance.
Bill Maiola passed away in February 2016, ever optimistic and looking for new solutions even in his final days. Today his head cheerleader plans to carry out his wish to raise $1 million for lung cancer research. “It’s an opportunity to show how much we loved Bill and to make a difference.”
To learn more about the Maiola Family Fund for Lung Cancer Research, contact Jennifer Daly at 404-778-4270.
Winship Magazine | fall 2016 21
Bill and Grace Maiola started a fund to support lung cancer research.
WHY I RUN
BY Marlene Goldman
SURESH RAMALINGAM 6 YEARS RUNNING
One sweltering day this past June, Sanjith Ramalingam, age six, and his brother Rohan, 10, set up a stand at a community swim meet to sell lemonade and spread the word about the Winship 5K. They raised $75 for research that day and boosted awareness of the event that they’ve participated in since its inception.

It’s a family affair for even the littlest Ramalingam, who ran the “Trot for Tots” race at the inaugural Winship 5K.

“We have all felt the pain caused by cancer to members of our family and friends,” says Winship Deputy Director Suresh Ramalingam. “We run because we believe that as a community we can beat cancer and make a difference in patients’ lives.” Fondly known to his patients as Dr. Ram, he runs the race with his wife Selvi and the boys.
Supporting the 5K is a step in the right direction. Proceeds support exciting research ideas that need pilot
funds to support the initial work before it can get substantial backing from major funding sources. Ramalingam points to researchers like Adam Marcus who, thanks in part to Winship 5K seed money, secured major grants from the National Cancer Institute to fund his research into a gene suspected of making many types of cancer cells metastasize.
This year, the 5K took on an even more personal note for Dr. Ram and many of his Winship colleagues who walked or ran in honor of a fellow physician currently battling cancer.
“There’s nothing more inspiring than to see patients, family members, friends, and Winship members walk for a cause that is bigger than any of us.”
JONI PAYNE YOUNG 4 YEARS RUNNING

Joni Payne Young runs for her “steel magnolia”—her mother who, since 2004, has faced breast cancer and renal cell carcinoma that spread to her brain and lungs. “It’s been a marathon,” her daughter says, “but she’s an amazingly tough lady.”
When Judy Storey Payne lost her kidney to renal cancer in 2004, she needed an activity she could do sitting rather than standing during her long recovery. Daughter Joni gave her watercolors. That art therapy resulted in a series of vibrant paintings, including a magnolia that graces the thank you notes Young sends to the many people who
22 Winship Magazine | winshipcancer.emory.edu
feature | the winship 5k
One-year old Sanjith Ramalingam got a helping hand from dad and big brother Rohan at the inaugural Winship Win the Fight 5K in 2011.
have supported her in the Winship 5K.
Young first learned about the race in 2013, immediately signed up, and raised $2,900 in just two weeks.
“I’ve never been comfortable asking for money but cancer is such an easy ask,” she says. “My grandfather died from cancer, I have sorority sisters fighting cancer as well as a fellow landscape architect who’s my age and who calls my mom his hero. So many people are impacted.”
Last year, Young raised more than $12,000 for the 5K, including a generous donation from a hometown friend who, noting that caregivers are often overlooked, made his gift in honor of Young’s dad.
For Young, the 5K is about funding research and believing that every step adds more time to a cancer patient’s life.
Research, she believes, has kept her mother alive with new treatments, including an immunotherapy drug just approved last November.

“When you can’t cure your loved one yourself, doing the 5K is really great therapy. The first year I was running for her life. My motivation now is that somebody did this so my mom could have the best treatment. I want to pay it forward for current and future patients.”
THE PINDERS 5 YEARS RUNNING
Anna Pinder cried the first time she and husband Steve crossed the finish line of the Winship 5K. It was fall 2012, one month into Steve’s treatment for Hodgkin lymphoma. “I was terrified and didn’t know what to expect.”
Steve Pinder had donated platelets for many years in response to a friend’s cancer. But on one visit to the Red Cross, his platelet count was elevated. Then he discovered a lump in his neck.
Life suddenly seemed out of control for the couple. Steve
began treatment. They put off starting a family.
They walked the Winship 5K that year, again in 2013, and in 2014, along with almost 200 colleagues, friends, and family. “I needed that 5K community,” Anna says. “There were so few things I could do to help
in Steve’s treatment. I wanted to support Winship because I was trusting them with my husband’s life.”
In 2015, they had another reason to celebrate: Anna was seven months pregnant. This year their daughter, Adelaide, joined them in her first 5K.
“I do the 5K because I want other people to celebrate being done with treatment and being able to move on with their lives. Steve and I are very lucky. He had a great response to treatment and now we are living our ‘happily ever after’ and raising our beautiful daughter. I want other people to be able to live their happily ever after too.”
ALIA CHERNNET
6 YEARS RUNNING
No matter where she is or what’s she’s doing, Alia Chernnet says she’ll walk or run in the Winship Win the Fight 5K every year for the rest of her life.
She had always been active and healthy, but just before her 23rd birthday, less than a year into her professional career, a distended abdomen prompted a visit to her gynecologist. In April 2011, surgeons removed a 5-pound ovarian tumor.

After four months of chemotherapy she spotted ads about the first Winship 5K. “I wanted to do something
to make me feel normal,” she says. So she walked the 5K with her two brothers and two friends that year. In 2016, she celebrated her fifth year in remission with her 30-plusmember team—the Abyssinian Warriors, aptly named after the East African region now known as Ethiopia where her family came from and which has never been conquered.
“When I was sick, even getting out of bed or walking was a challenge,” she says. “If I can walk for somebody else now, that means the world to me. Every dollar goes to research. I would never want my brothers or my children to go through what I had to go through. I want to be part of the genera-
tion that helps find a cure.”
The best part of the race, she says, is when she joins other survivors for a photo. “I can see from year to year how far we all have come and I am humbled by the experience.”
Winship Magazine | fall 2016 23
WHEN CANCER COMES BACK
Wendy Baer is medical director of Psychiatric Oncology at Winship, where she helps patients and their families deal with the stress of receiving a cancer diagnosis and subsequent treatment. She believes strongly in the team approach and collaborates regularly with the doctors, nurses, and social workers that make up a patient’s care team.
RECENTLY, A PATIENT I’ll call him John—who had just completed chemotherapy for lymphoma came in for his mental health appointment with three questions written down on a piece of paper.

1. How do I go on living knowing that my cancer could come back at any time?
2. Should I change my job?
3. How do I control my worry about the next set of labs and CT scans?
24 Winship Magazine | winshipcancer.emory.edu point of view
John’s questions are common for a cancer survivor; asking them out loud and getting mental health care to address his anxiety showed courage. While there is not one right answer to each question, the questions provide a framework in how to think going forward with life after cancer treatment, and how to cope if cancer comes back.

At the end of treatment, everyone hopes that cancer is gone, forever. However, recurrence is a reality for many people and few things are as discouraging as having cancer come back. Just when you thought you could focus on work, friends, travel, now you are back getting scans, blood draws, and meeting with doctors. I advise people at that vulnerable time to go forward with the goal of living well and making the most of today. That may sound simple, but if cancer teaches us anything, it’s the importance of not taking time for granted.
The first thing I remind people with recurrent cancer is that they have managed cancer before, so they can manage it again. Even if it doesn’t feel like it at the moment, they have coping skills. Just as they did the first time, they can sit down with a trusted family member and their medical team to make a plan for managing the cancer. Once there is a plan in place, most people feel much less anxious.
John had thought about changing his job because cancer made him realize “life does not last forever and things might change at any time.” He dedicated time to think about what he really wanted out of his life and realized that a more service-oriented job would be a better fit for him. Given his insurance benefits and financial situation, he decided to stay in his current occupation for the pres-
ent, but he signed up for evening teaching classes at a community college. His plan is to do some volunteer tutoring at a local middle school, then decide if he will make a career change to teaching. John actively decided not to let cancer stop him from a fulfilling career; rather, he used cancer as his springboard to think about and plan for meaningful work.
Should a cancer experience stop anyone from searching out their dream job? Absolutely not. The whole reason to fight cancer is to go on living as well as possible. The reality of cancer recurrence can be anxiety about follow-up scans and tests, poor sleep, irritability, and trouble concentrating. Stress management skills are critical during this time. I suggest patients do what they can right now to make themselves feel as well as possible. It may be as simple as taking time to get outside, buy fresh flowers, see a funny movie, listen to an old album, or have lunch with a friend.

John decided the best way to tolerate his return to the cancer center was to make plans for a fancy fish dinner the night before the appointment, “I’d much rather think about the ocean and seafood than lymphoma.”
I often urge people to not beat themselves up for what are very normal emotions and reactions. Worst case scenarios inevitably go through our minds because that’s how our minds are wired. So, let those thoughts come, notice them, take three long, slow deep breaths, and then let them go again. Next step? Make a plan….
Cancer should not invade every moment of the day. The goal is to contain cancer, not just physically, but mentally. Choose a time of day (mornings are best to protect sleep) to do all the calling, scheduling, worrying, and planning. After that, cancer thoughts and worries that come up during the day get stashed in a mental box and dealt with the next morning. Then, pay attention to small pleasures that have nothing to do with cancer. Knowing what matters to you and making the most of each day will mean that you are living as well as possible. W
Winship Magazine | fall 2016 25
Worst case scenarios inevitably go through our minds because that’s how our minds are wired. So, let those thoughts come, notice them, take three long, slow, deep breaths, and then let them go again. Next step? Make a plan….
KAY HINTON
ILLUSTRATION BY BRIAN STAUFFER


1365-C Clifton Road N.E. Atlanta, GA 30322 winshipcancer.emory.edu 1-888-Winship This is my legacy. Have you planned your legacy? giftplanning.emory.edu 404.727.8875 “MY CANCER DIAGNOSIS led to one of the most enriching experiences of my life because I was treated at Winship Cancer Institute. Not only have I remained cancer free for ten years, but I’ve gained a second family through the meaningful connections I made with doctors, nurses, and staff. They shared conversation, laughter, and even meals with me. Leaving my estate to Winship for cancer research is the best decision I’ve made. My gratitude is endless.”
Printed by an FSC-certified printer using sustainable methods that reduce waste and volatile organic compound (VOC) emissions. Paper is a 50% PCW recycled sheet, sourced from a certified managed forest
Edye Bradford Clayton, Georgia














 By Catherine Williams
By Catherine Williams



 BY Quinn Eastman
BY Quinn Eastman


















 CASSIE MITCHELL PARALYMPIAN, BIOMEDICAL ENGINEER
CASSIE MITCHELL PARALYMPIAN, BIOMEDICAL ENGINEER

















