I feel like I was very lucky, honestly. I thought, wow, if this is cancer, I’ve got the right treatment.
Tom's Doctor
-
Mehmet Asim Bilen, MD Director, Genitourinary Medical Oncology Program

The first time Tom was diagnosed with kidney cancer, in 2016, he had to have one of his kidneys removed. Then when he was diagnosed again the following year — his disease spread to distant sites — doctors at Winship Cancer Institute of Emory University recommended that he consider enrolling in a clinical trial.
Tom enrolled in a clinical trial of an immunotherapy testing whether adding a second agent might increase its effectiveness. Tom recalls being immediately interested in the prospective trial, noting that the late President Jimmy Carter also had been treated with the same immunotherapy. “There was already positive information out there about President Carter’s care, and if I could get the same thing that he did, of course I would be interested. My thought was that one more helpful drug is not going to hurt anything. And that’s how it started.”
The clinical trial Tom participated in was led by medical oncologist Mehmet Asim Bilen, MD, director of Winship’s Genitourinary Medical Oncology Program and associate professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine. Bilen described the process by which patients are invited to participate in a clinical trial.
The first step in determining a patient’s eligibility for a clinical trial is to ascertain the patient’s diagnosis and cancer stage. Bilen explains the diagnosis, outlines the standard of care and discusses how the proposed treatment works, including potential side effects. If a clinical trial is a possibility, he walks the patient through what the trial involves: its design, the drugs being tested, their potential risks and benefits and how it compares to standard treatment.
“I put those side by side and we have an in-depth conversation,” Bilen says, “because the more a patient understands their options, the potential benefits and possible side effects, the easier it is to make a decision. From there, if they’re interested in participating in a clinical trial, I always ask them to go back home, think about it and discuss it with their family and friends. Most come back with more questions which we discuss. Once they are comfortable and certain about their decision, we move forward.”
Testing tomorrow’s treatments today

Tom during a visit to Winship's Phase I Clinical Trials Unit in 2019.
Ajay K. Nooka, MD, MPH, is Winship’s associate director of clinical research, director of the Myeloma Program and a professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine. He provides strategic oversight for Winship’s clinical trials portfolio, with a focus on ensuring high-quality, safe and ethical research and equitable access to innovative trials.
Nooka points out that today’s standard of care treatments were once part of clinical trials. “They didn’t just appear from thin air.” He explains, “They were compared to what was a standard of care at the time. When a newer treatment proves superior, it becomes the new standard of care.” That’s why clinical trials matter, he says. “We are evaluating newer treatments that have the potential to be more effective. However, we do not know that yet. That’s exactly why the clinical trial is being done.”
More than a thousand Winship patients participated in an interventional clinical trial in 2024. Winship offers the most cancer clinical trials in Georgia, with 550 open interventional trials in 2024. “There is a clinical trial for nearly every type of cancer,” says Nooka. “The trials help determine which approach is better, the current standard of care treatment or the newer treatment that we’re evaluating in the trial.”
Nooka says that for patients, participating in a clinical trial is a “win-win situation” because, even in a randomized trial, “you’re not getting anything less” than what you normally get. You receive either the standard of care or the new treatment being tested. “There is a potential that you could get a new treatment that’s better than the existing standard of care.”
Misunderstanding of what is entailed in a clinical trial can keep some people from participating in one. “People come with a stigma that clinical trials are ‘experimental,’” says Nooka. “But not all clinical trials are the same. This is not experimenting for the sake of experimenting—it’s structured, closely monitored, highly regulated and ethical research.”
Another concern people bring is whether their insurance will cover the cost of participating in a clinical trial. Nooka explains that insurance still covers the costs of the standard of care treatment, less any copays for which the patient may be responsible. Any costs related to the clinical trial are covered by the trial itself. “So, whether or not you participate in the trial,” he says, “if the standard of care means coming in once every three months, insurance covers that visit. In the clinical trial, if you’re asked to come four times, the clinical trial is going to cover those additional visits. The patient should not be upcharged or billed unnecessarily.” When someone participates in a clinical trial at Winship, Nooka says, “there’s a lot of transparency from our perspective.”
To help patients navigate the decision, he advises patients to ask questions. “Be vigilant, ask whether there are options beyond the standard of care.” Weigh the benefits and risks of participating in a clinical trial. What are the possible advantages or concerns? Is the required schedule of visits feasible for you? What’s the potential upside or downside?
Nooka adds, “The treatments being tested in clinical trials today are tomorrow’s standard of care treatments.”
Nothing less than standard of care
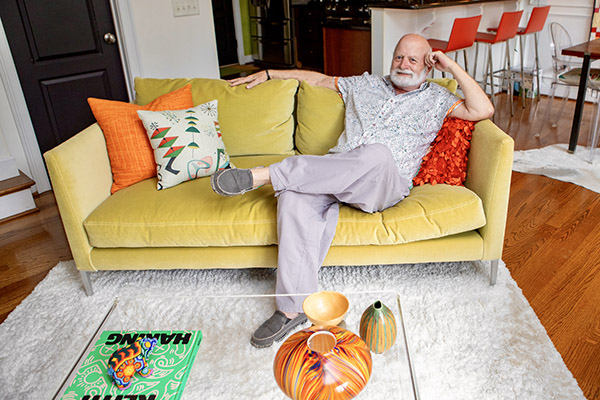
Tom relaxing at his home in 2025.
Bilen agrees it’s essential for patients to understand that in a clinical trial they are not getting anything less than the standard treatment. “They’re not getting anything less, but they may be able to get something in addition to what’s standard of care,” he says. He notes that in the clinical trial Tom was getting an immunotherapy agent that was standard of care plus another immunotherapy agent.
Within a few months of joining the clinical trial, Tom experienced extremely positive outcomes. “I started responding positively to the treatment right away,” he says. After about five months, “they were saying, wow, you really are moving along.”
Bilen says, “Overall, we are very, very pleased to see that he had a fantastic response after he participated in the clinical trial. After we started the treatment, he achieved a complete response. That means imaging no longer showed signs of cancer.”
After two years of follow-up therapy, Bilen says, “we were able to stop the treatment. He still comes to see us for long-term follow-up with imaging and blood work, but he’s been cancer-free now for many years—which is a huge achievement. Now maybe ‘cure’ is what we are thinking.”
Says Tom, “They started calling me their poster child because they said, ‘You have done well with treatment for the disease spread to distant sites and responded so positively, so quickly.’”
There were side effects of the treatment—fatigue, some skin problems, stiffening in his hands and feet. But Tom says his appetite was always good and he never felt nauseated. Despite these temporary side effects during treatment, Tom is pleased by his overall experience with immunotherapy and in the clinical trial. “If anybody can have immunotherapy, that would be my recommendation if you have an option. I feel like I was very lucky, honestly. I thought, wow, if this is cancer, I’ve got the right treatment.”
He speaks in similarly glowing terms about the clinical trial staff, particularly the nurses. “They were a godsend,” he says, adding that their emotional support and enthusiasm helped him persevere. “You’re never left on your own.”
Looking back, Tom reflects positively on his decision to join a clinical trial. “The cancer was gone, knock on wood. That was in 2019, and now it’s 2025. I’m doing great!”
Care tailored to your needs
Care for patients with kidney cancer at Winship includes leading cancer specialists collaborating across disciplines to tailor treatment plans to each patient’s needs; innovative therapies and clinical trials; comprehensive patient and family support services; and a care experience aimed at easing the burden of cancer.