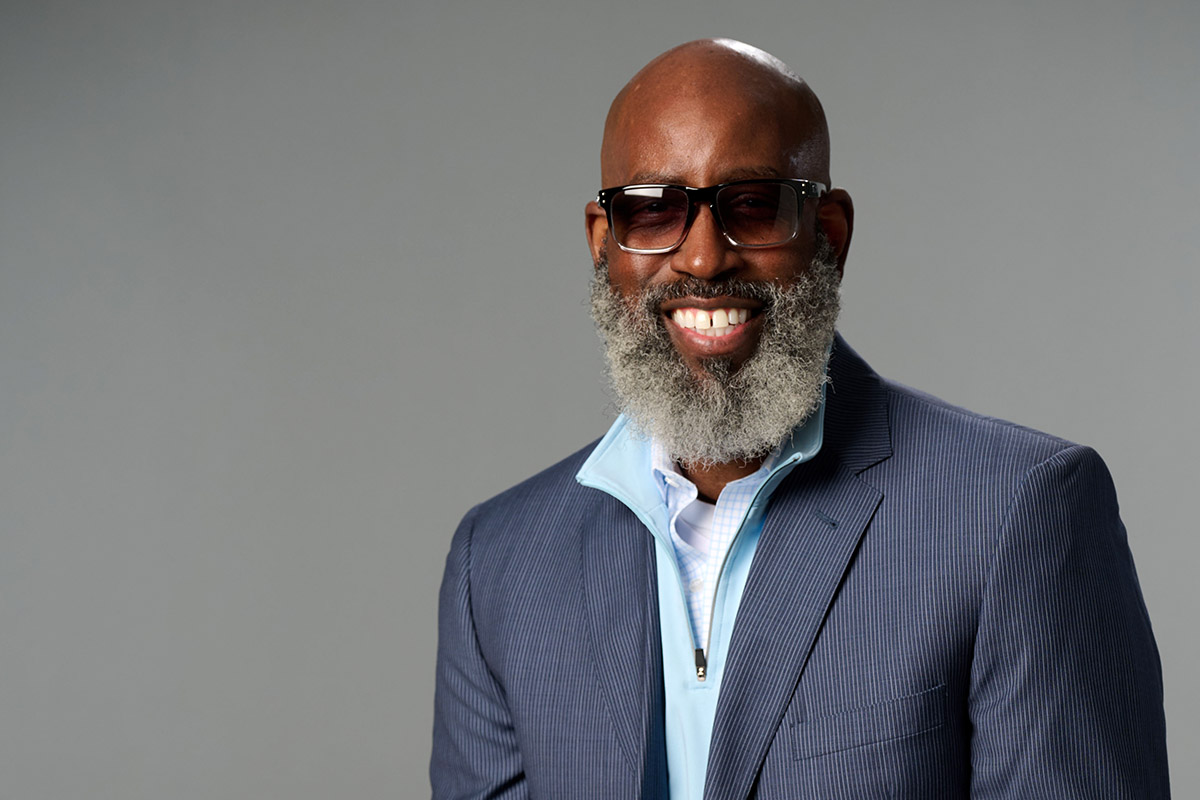
Through the entire process, it felt like I had a team rooting for me to win — versus just going through procedures and going through the motions.
In late 2013 Christopher kept getting sinus infections in the left side of his nose, making it hard to breathe. His general practitioner prescribed antibiotics and told him it would clear up. “And it would never clear up,” he says.
As Christopher and his family were getting ready to visit a museum on his daughter’s sixth birthday, he blew his nose. Instead of “your normal runny nose,” there was blood. Back he went to his general practitioner. This time they referred him to an ear, nose and throat specialist who thought Christopher had a sinus polyp. There was even more blood when the doctor biopsied it.
Christopher knew something was seriously off when the doctor called him two days later and told him to sit down. "You have cancer," the doctor told him.
Cancer was already too familiar in Christopher’s family after his eldest brother died from leukemia. “But for me, that was pretty shocking because I didn’t have any symptoms or anything like that.” The doctor told him, “This is beyond my scope to manage” and referred him to a surgeon at Emory Healthcare.
The cancer Christopher had is known as sinonasal intestinal type adenocarcinoma (ITAC), an epithelial tumor of the nasal cavity and paranasal sinuses. It’s often related to professional exposure to organic dust such as wood or leather and resembles intestinal adenocarcinoma in that a feature of it is an increased production of mucin, a component of mucous that protects tissue.
The treatment plan

The initial treatment plan was surgery. “I had surgery soon after my first visit with the surgeon,” Christopher says. “At the time, I didn’t realize how fast tumors can grow. I had no idea.” He says it was less than two weeks between his initial visit and surgery by renowned sinus surgeon John M. DelGaudio, MD, director of Emory Sinus, Nasal, & Allergy Center and professor and vice chair in the Department of Otolaryngology at Emory University School of Medicine.
For two to three months afterward, Christopher recovered from the surgery. He returned for checkups, rinsed his sinuses as directed and made sure to keep the surgical area clean. But while on a business trip to Ohio, “a very similar thing happened again,” he says. “I couldn’t breathe, and then I blew my nose and there was a similar discharge.” Christopher says his first thought was, “Oh, this is weird.”
At that point, Christopher’s case went before the tumor board at Winship Cancer Institute of Emory University. The board is a multidisciplinary team of experts in particular types of cancer who meet regularly to discuss cases, collaboratively develop individualized cancer treatment plans and discuss eligibility for clinical trials. They recommended that Christopher receive several rounds of chemotherapy and radiation therapy to help shrink and eliminate the tumor and then reassess his case.
Given the seriousness of his situation, Christopher sought a second opinion at Johns Hopkins in Baltimore. “I also did my own research into Emory as well,” he says, “just in terms of the background of Winship and historically how cases turned out, how patients were treated.”
Based on the information he gathered, Christopher concluded, “I just knew that I would get the best treatment at Winship.”
What he liked best at Winship

Christopher on his bicycle
“One thing I love about Emory is their candidness,” Christopher says. He describes how during his seven weeks of getting chemo and radiation treatment at the same time, his care team told him that while his tumor had been reduced, increasing the levels of treatment offers “a better chance of us really nailing and getting rid of the entire tumor—but there will be degradation to your eye.” The other option was to keep the treatment levels as they were, “but there may be a risk of cancer remaining or recurring.” He says they were surprised when he told them to “give me the highest grade levels you have, and we’ll go from there.”
Afterward, Christopher says he was talking with his father who asked, “Well, Chris, why did you do that?” To which he responded, “Well, Dad, it’s kind of an easy decision. Either you lose your eye, or you lose your life.” He said that if he hadn’t gone ahead with agreeing to the increased treatment levels, and the tumor came back, he would always wonder if he should have made the decision that he did make.
“Emory didn’t have to tell me about the risk,” Christopher says. “They could have just increased my treatment levels. I would have never known. But they told me the risks, and I think that’s the one thing that patients often don’t put a lot of stock in is understanding the risks they’re going through and that doctors communicating that risk is to help you make the best decision.”
For Christopher, this communication from his care team—laying out the potential risks—was uniquely important. “The thing that was unique was the fact that the risk was expressed and they gave me time to think about it. And I was all in. I leaned into ‘If we’re going to do it, let’s do the best we can, the most we can.’ That way if it came back, I know I did all I could do.”
The other thing Christopher says he loved about Winship was that “through the entire process, it felt like I had a team rooting for me to win—versus just going through procedures and going through the motions.” He recalls his final chemotherapy treatment. “They have a bell to ring when you get through the end of treatment. At the bell ringing, I did the hammer dance and the moonwalk. My wife recorded it, and it was the happiest day getting through all of that.”
More than five years after his “cancer event” as he calls it, Christopher is doing well. “I’m fully healthy, knock on wood,” he says. He bikes about 100 miles a week—a result of his cancer experience, he says. “My thought process was in case it ever came back, I wanted to be as healthy as I needed to be to fight it again.” He also bikes because it’s what he loves to do. Same with helping care for his parents who are in their eighties. And he volunteers in Emory’s Eye Center.
Christopher offers anyone facing cancer his own hard-earned insight: “I think oftentimes when you hear the word cancer, you automatically think the worst, and sometimes the worst happens. But if you have a team here at Winship that can help you fight through it, you’d be surprised what you can beat.”
Care tailored to your needs
Care for patients with head and neck cancer at Winship includes leading cancer specialists collaborating across disciplines to tailor treatment plans to each patient’s needs; innovative therapies and clinical trials; comprehensive patient and family support services; and a care experience aimed at easing the burden of cancer.