Welcome to Winship
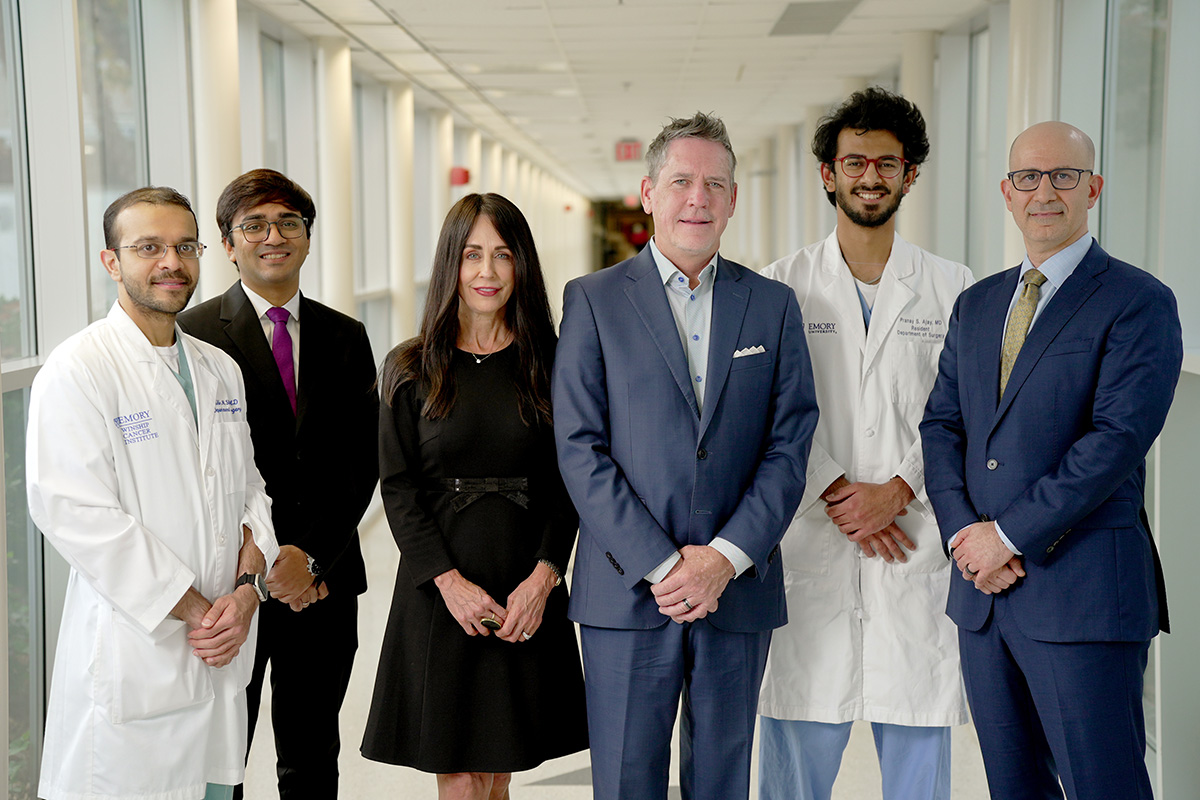
Meet four of Winship’s outstanding research scientists whose day-to-day work is changing the game in important ways for people with cancer.
David S. Yu, MD, PhD
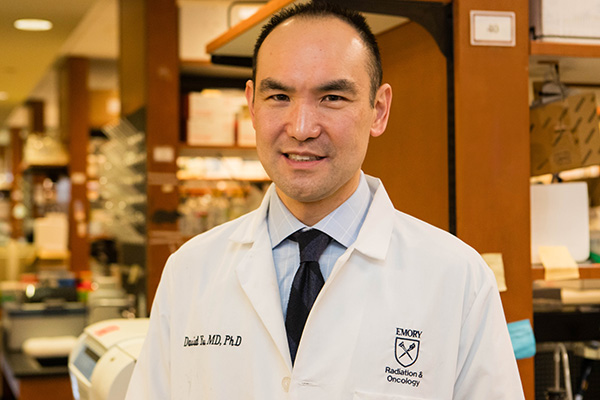
David S. Yu, MD, PhD
Photo: Jenni Girtman
Yu is a member of the Cell and Molecular Biology Research Program at Winship Cancer Institute and a radiation oncologist specializing in head and neck, breast and lung cancers at Grady’s Loughlin Radiation Oncology Center. Yu, MD, PhD, holds the Jerome Landry, MD, Chair of Cancer Biology and is a professor, director of the division of cancer biology and vice chair for biology research in the Department of Radiation Oncology at Emory University School of Medicine.
Q: What is an example of how you have translated insights from interacting with patients and lab researchers to innovative therapies, and how have those therapies improved the quality of life for people with cancer?
A: In collaboration with Winship researcher Baek Kim, PhD, we have found a novel role for cellular enzyme SAMHD1 as a DNA repair factor that mediates resistance to DNA damaging agents, such as radiation therapy, in breast cancer and other cancer types. Interestingly, this same cellular enzyme is well known for preventing HIV infection. Vpx, a protein that supports HIV-2, degrades SAMHD1. We exploited this natural way for HIV-2 to degrade SAMHD1 by packaging Vpx in virus-like particles. We showed that these particles can degrade SAMHD1 in breast cancer cells and tumors and can make cancer cells and tumors vulnerable to radiation therapy.
Q: What are you most excited about?
A: We are investigating our strategy of using the virus-like particles containing Vpx to help stem-cell-like CD8+ T cells mature. These cells then kill infected or malignant cells and make it possible to treat breast cancer with immune checkpoint inhibitor therapy. This enables the body's natural defenses to recognize and attack cancer cells more effectively.
Tyler S. Beyett, PhD
Tyler S. Beyett PhD
Photo: Jenni Girtman
Beyett is a member of the Discovery and Developmental Therapeutics Research Program at Winship Cancer Institute and an assistant professor in the Department of Pharmacology and Chemical Biology at Emory University School of Medicine. His research is primarily focused on the clinical development of allosteric EGFR inhibitors for drug-resistant lung cancers, and his lab is generally interested in kinases and phosphatases.
Q: Your research is primarily focused on the clinical development of “allosteric EGFR inhibitors” for drug-resistant lung cancers. What are these and why are they important for lung cancer?
Q: Your lab is also interested in studying kinases and phosphatases. What are they and what are their normal roles compared to what happens to them in cancer?
Xu Ji, PhD, MSPH
Xu Ji, PhD, MSPH
Photo: Jenni Girtman
Ji is a member of Winship’s Cancer Prevention and Control Research Program and an assistant professor in the Department of Pediatrics at Emory University School of Medicine. Her research focuses on leveraging her quantitative research skills and theoretical grounding in health services research for improved pediatric cancer care and cancer survivorship.
Q. Why are big data analysis, administrative data, data linkage and statistical modeling important for pediatric cancer care and survivorship?
A: The novel linkages and statistical application of population-based data (e.g., administrative insurance records, medical records, cancer registries, geospatial data) allow the generation of rigorous, realworld evidence pertaining to the gaps in health and health care after a diagnosis of pediatric cancer. Such evidence informs new interventions in clinical practice and health policy changes designed to improve the lives of people with, and survivors of, pediatric cancer.
Q. How you are able to leverage your quantitative research skills and theoretical grounding in health services research to benefit pediatric cancer care and survivorship?
A: To launch my research career in pediatric cancer care and cancer survivorship, I received internal funding that allowed me to analyze administrative Medicaid data to examine insurance issues among pediatric cancer survivors. We found that a substantial proportion of survivors (ranging from 24% to 47%, depending on the specific survivor cohort under study) were insured with Medicaid. Among these, over one-half experienced gaps in Medicaid coverage and in their care. These gaps were associated with inferior cancer outcomes compared to those with private insurance or uninterrupted Medicaid. In one study, my colleagues and I linked Medicaid insurance data to the established cohort from the Childhood Cancer Survivor Study, a retrospective cohort of 30,803 adult survivors of pediatric cancer recruited from 30 institutions across the U.S. who were diagnosed between 1970-1999. We used the linked dataset to quantify patterns of health care utilization among Medicaid-insured survivors, overall and by sociodemographic groups, following Medicaid expansion under the Affordable Care Act.
Sarwish Rafiq, PhD

Sarwish Rafiq, PhD
Photo: Jenni Girtman
Rafiq is a member of the Cancer Immunology Research Program at Winship Cancer Institute, program leader for Winship’s CAR T Basic/Translational Research and an assistant professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine. She is a translational research scientist with a broad background in the preclinical development of immune-based treatments for cancer.
Q: Why is immunotherapy such a powerful approach to treating cancer?
A: The immune system is the body’s natural defense mechanism against infections and diseases such as cancer. However, cancer cells often develop mechanisms to evade detection by the immune system. Immunotherapy aims to boost the body’s immune response against cancer. There are many advantages to this approach. Immunotherapy can be more precise and target cancer cells specifically while sparing normal, healthy cells. Furthermore, this type of treatment can create a lasting effect on the immune system, called immunological memory, wherein immune cells may continue to patrol the body, recognizing and eliminating cancer cells even after the initial treatment. Finally, as the immune system is highly dynamic and can evolve to recognize new threats, immunotherapy has the potential to adapt to changes in cancer cells to avoid resistance to treatment.
Q: What obstacles remain in expanding CAR T technology for more widespread use in cancer?
A: CAR T-cells are a type of treatment in which a patient’s T-cells (a type of immune system cell) are changed in the laboratory so they will attack cancer cells. Although CAR T-cells have been remarkably effective against certain types of blood cancer, expanding the number of patients who can benefit from this therapy faces challenges. First, the process of engineering personalized T-cells for each patient is complex and resource-intensive. High costs can limit accessibility, making it challenging for many patients to afford this treatment. The time it takes to manufacture CAR T-cells can also be a challenge. In some cases, patients with rapidly progressing cancers may not have enough time to wait for the production of personalized CAR T-cells. Current research is looking at ways to create a more “off-the-shelf” CAR T-cell product that can be universally used in patients. Finally, CAR T-cells can be suppressed in the microenvironment of tumors, especially for solid tumors. Maintaining or boosting their efficacy here is an active area of research.